In the field of psychiatry, as in any medical
specialty, patients are given diagnoses. In this post I will discuss what I believe to be the positive and negative consequences of assigning diagnostic labels.
I hate to start this way again but I must begin with disclaimers….
- This is not a scholarly blog. I could, of course, dust off my graduate school textbooks to reference others' work that supports my opinions, but I think that would bore us both. However, I am willing to direct you towards sources if you contact me with questions.
- This post is full of my personal opinions, but I feel I have something to offer the debate given my education (BA in psychology and MA in counseling) and my work as a counselor in the mental health and substance abuse fields. I have not been in the field long, having started graduate school in 2007, but I have had much face-to-face interaction with patients, families and health-care providers.
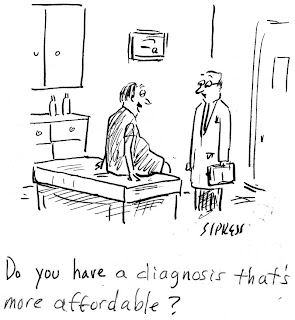
- I found all the images in this post on the internet, and I hope you find them amusing and not offensive :)
Background information: Physicians use the Diagnostic and Statistical Manual of Mental Disorders (DSM) to diagnose mental illness. Currently used is the text-revised 4th edition published in 2000 by The American Psychiatric Association. The fifth edition is scheduled to come out next year (exciting!).
Alright, let's get started.
Diagnostic Labels: The Good and the Bad
No one (I hope) would consider it harmful to
diagnose someone with high blood pressure or diabetes. Why? Diagnostic labels provide a "common language," inform treatment and ensure insurance reimbursement for services.
By a "common language" I mean that much is communicated in only a few words. Inherent in a label is a specific collection of symptoms. It would take much longer for one to describe a patient's life in detail, whereas a label allows healthcare and insurance providers to quickly and efficiently communicate what one believes to be the current problem.
By "informing treatment" I mean that labels instruct healthcare providers on how to proceed. Of course, given a specific diagnosis, not all doctors will make the same decisions. But associated with each diagnostic label are lists of things that one should NOT do and a list of interventions which have proven effective in treating others who have received the same diagnosis.
Diagnostic labels are needed for securing insurance coverage. A third party will not pay for treatment if a problem has not been identified and recorded. This consequence of psychiatric labeling, though straightforward, is extremely important; healthcare is expensive.
Well that sounds great, no? If multiple individuals involved in a patients care (not limited to healthcare and insurance providers, this group may also include family members, courts and schools, among others) can communicate quickly and efficiently, insurance coverage for treatment is secured, and inherent in labels are treatment recommendations, what is the downside? I find it hard to identify negative consequences for diagnosing someone with diabetes; the label facilitates treatment. So why are psychiatric (mental illness, mental disorder) diagnostic labels different?
First, psychiatric diagnoses are subjective. Unfortunately there are no blood tests for mental illness. Brain imaging is becoming more and more sophisticated, and some differences have been noted in the brains of the mentally ill, but brain imaging currently cannot inform diagnosis. Physicians rely solely on self-report. This data can include reports from others too (family members, teachers, therapists, work supervisors, etc.) but is still biased information. Therefore the risk of misdiagnosis is higher in psychiatry than in other medical specialties. As you may guess, the consequences of misdiagnosis can be severe. For example, misdiagnosing a person with bipolar disorder with depression alone can lead to prescribing an antidepressant medication (without an accompanying mood stabilizer), which can then induce a manic episode.
Additionally, interpersonal factors influence diagnosis. Building a trusting relationship with patients is essential as a psychiatrist because you rely upon the patient disclosing sensitive (painful, shameful, embarrassing, etc.) information for diagnosis. If a patient shares different information with different doctors because of social reasons (trust, competency beliefs, paranoia, likability, prejudice, etc.) he may receive different diagnoses. In psychiatry, interpersonal factors have greater influence on diagnosis than in other medical fields, where objective data and "hard facts" are the principle determinators of diagnosis.
Not only is the risk of misdiagnosis high in psychiatry, but, in our current fast-paced and fee-for-service healthcare system, physicians often feel pressure to diagnose quickly. After all, insurance companies will not pay without a label on file. Quick diagnosis can be helpful in that, if accurate, treatment can begin immediately and help the patient. The DSM provides neatly constructed check-lists for the diagnostic process. Yet spending more time eliciting a detailed history of the presenting symptoms and simply trying to see the “full picture” of the patient’s life will most certainly lead to a higher incidence of accurate diagnoses. But who has the time? Words are needed on paper or treatment will not be initiated. Therefore postponing diagnosis can cause harm, but diagnosing quickly increases the risk of misdiagnosis. I do not blame doctors for the problems inherent in rapid diagnosis, they must operate under factors beyond their control, and of course, just want to help their patients. Many people, consciously or not, make a value judgment when they see or hear a psychiatric diagnosis.
The medical model, on which the DSM-IV is
based, assumes biological causes for mental illness. In accepting the medical model in psychiatry one is operating under the belief, that, like any other illness, the sufferer has limited control over his or her health. In other words, he cannot become well by willpower alone. One of the reasons psychiatric labels are damaging is because of the widespread
belief that individuals can “will” themselves out of mental illness. I sometimes call this the “get over it” and “just work harder” view. Psychiatrists (I hope)
are not passing judgment on the individual’s character when assigning a label but rather making inferences as to
what biological functions are causing symptoms. A person is stigmatized when others equate psychiatric diagnoses with weakness or a lack of personal responsibility.
However, symptoms of many mental illnesses can be mitigated by lifestyle change. Examples include altering one’s diet, engaging in
regular exercise, keeping regular sleep patterns, and even gaining exposure to UV light! Another negative consequence of labels may therefore be learned helplessness. A patient may
conclude that managing their illness is entirely beyond their control since it is caused by their biology rather than
their behavior. Labels can thus be used as an excuse to keep old habits.
* It is important to
remember that one cannot cure their
illness through lifestyle change, only manage symptoms.
Perhaps, having read this far, the diagnostic process in psychiatry seems hopelessly messy and confusing. I have good news. Surprisingly, despite the problems discussed above, the small collection of words that constitutes a psychiatric diagnosis can bring hope, relief and comfort to patients and their families.
Families of individuals with mental illness may feel hopeless, confused and angry. Not only is the the behavior of their loved ones inexplicable and scary, it can also be extremely damaging to relationships. For example, it's difficult to "pick up where you left off" following a suicide attempt. A label provides relief because one learns that other individuals have acted in similar, inexplicable ways. So many others, in fact, that the collection of behaviors has a name! Along, with that name, as discussed above, are recommendations on how to proceed with treatment. Therefore, a diagnosis can supply hope that things can change.
Most psychiatric symptoms are not "pretty" and the mentally ill are stigmatized and misunderstood. It makes sense, therefore, that families would wish to keep private whatever shameful and embarrassing things their loved one is doing. They may withdrawal from activities and relationships and begin to feel alone in their suffering. A diagnostic label can reduce this sense of isolation; now they know that other families face similar challenges.
Families may gain empathy for their loved one following diagnosis. They can now view hurtful behavior as a symptom of an illness rather than a personal attack. When one understands that the mentally ill have limited control over their actions (when symptomatic) it becomes easier to forgive and rebuild relationships.
I have talked much about how labels help families. Yet diagnostic labels can benefit patients for all of the same reasons.
It is terrifying and confusing to feel as if you do not have control over your own behavior, or that you do not perceive reality as others do. Understandably, you may feel scared, alone and hopeless. A diagnosis can reduce the sense of isolation because you learn that others have experiences similar to yours. It can provide hope because you learn that others have responded to treatment. You can gain empathy for yourself, which is an awkward way of describing self-acceptance (not denying responsibility for behavior, but rather learning to be less self-critical). Most importantly, in my opinion, a diagnosis helps everyone look to the future. Lets examine the past to arrive at a diagnosis, and then use that diagnosis to move forward.